RFA Treatment of Perforator Veins
RFA treatment of perforators is a minimally invasive method aimed at closing incompetent perforator veins in chronic venous insufficiency. With radiofrequency energy, the vein wall is heated and deliberately ablated, preventing reflux. In this way, venous pressure decreases and symptoms significantly improve.
RFA application in perforator vein insufficiency is also an effective solution particularly in cases with venous ulcers and skin pigmentation changes. The procedure is performed under ultrasound guidance and local anesthesia. Once the vein is closed, backflow in the superficial veins is prevented and the healing process accelerates.
Advantages of radiofrequency ablation include a low complication rate, short recovery time, and preservation of cosmetic outcomes. Compared with open surgery, it causes less tissue damage. Patients are generally discharged the same day and can return to daily activities in a short time.
During the follow-up after RFA, the use of compression stockings and regular Doppler ultrasound checks is important. This ensures the durability of vein closure and helps prevent the development of new reflux. Appropriate patient selection and an experienced physician are the key factors determining the success of treatment.

Chronic Venous Disease (CVD) is, in the simplest terms, a persistent elevation of pressure (venous hypertension) within the leg veins. This continuously high pressure disrupts the structure of the vein walls, leading to dilation and failure of the valves to close completely.
In advanced stages of the disease (CEAP C5–C6), that is, at the stage of healed or active wounds (venous ulcer), these “incompetent perforator veins” (IPVs) play a critical role. Think of them as “faulty emergency exits” between the deep and superficial systems. While they should normally function in only one direction (inward), when pressure in the deep system rises excessively, these doors fail and begin to open in the opposite direction (outward).
In this situation, the high-pressure blood generated within the muscles (especially during walking) is “jet-washed” directly into the superficial system under the skin through these faulty perforator veins. This causes severe, destructive pressure in the subcutaneous tissues particularly on the lower–inner leg, in the area around the ankle known as the “gaiter zone.”
The consequences of this high pressure are serious. Vascular permeability increases and red blood cells begin to leak out of the vessels. The body cannot clear the iron (hemosiderin) from these leaked cells, and this iron accumulates under the skin, causing the area to take on a permanent brown-purple discoloration—almost like “rusting.” This constant pressure and leakage impair skin nutrition and trigger a chronic inflammatory reaction. The skin hardens, thickens, and loses elasticity (lipodermatosclerosis, C4b). This is a harbinger of venous ulcers (active wounds) that may open with even minimal trauma or spontaneously.
The “gold standard” for diagnosing perforator vein incompetence is Color Duplex Ultrasound (DUS) (color Doppler sonography). Beyond visualizing the structure of the veins with sound waves, this device produces a dynamic “flow map” that shows the direction, velocity, and volume of blood flow.
There have traditionally been certain criteria used to define a perforator vein as “incompetent” or “faulty.”
However, in modern venous disease management—especially when advanced disease (C5–C6, i.e., the ulcer stage) is in question—a factor far more important than rigid numbers is: localization.
Evidence-based data show this: even if a perforator is thinner than 3 mm, if it opens directly beneath the bed of an active venous ulcer (right under it) or feeds prominent varices in that region, it is considered clinically “significant” and requires intervention.
In other words, in advanced disease, the decision prioritizes the relationship of the vein to the ulcer and its hemodynamic impact (pressure it creates) on that area rather than its diameter in centimeters. The aim of treatment is to identify and eliminate the specific “high-pressure leak point” that prevents ulcer healing.
The primary clinical rationale for intervening on perforator veins is to halt and improve skin damage (pigmentation, induration) caused by advanced venous disease and, most importantly, to accelerate the healing of active venous ulcers (C6).
Typically, if a patient has reflux both in a main superficial vein (e.g., saphenous vein) and in perforators, treatment usually starts by closing the main superficial vein. However, if “stubborn” (refractory) ulcers do not heal despite this, or if ultrasound clearly shows that the ulcer is directly fed by a perforator, ablation (closure) of that perforator becomes a critical component. Treatment guidelines also explicitly state that hemodynamically significant—i.e., refluxing and causative—IPVs should be treated.
In the past, the traditional surgical method used to treat these faulty perforators was “Subfascial Endoscopic Perforator Surgery” (SEPS). Under general anesthesia, instruments and a camera were inserted through incisions in the leg to locate and ligate or divide these veins beneath the fascia (muscle sheath).
However, this approach created a serious dilemma. While treatment guidelines say “Treat these veins,” they also strongly state that SEPS—the traditional surgical method—should “never be performed” in those who need it most (advanced stage C5–C6 patients) due to its “high risks” (morbidity).
Why? Because SEPS is a surgery with a “high complication rate.” In these patients, whose skin is already damaged, prone to infection, and poorly nourished, making large surgical incisions can lead to wound-healing problems, severe infections, and prolonged hospitalizations.
This created a “treatment gap” for clinicians: there is a pathology (IPV incompetence) that needs to be treated, but the traditional surgical method (SEPS) is unacceptably risky.
This is exactly where minimally invasive endovenous (intravascular) techniques such as percutaneous, ultrasound-guided radiofrequency ablation (RFA) come into play.
RFA achieves the goals of the treatment guidelines by precisely closing the target IPV without the surgical risks caused by SEPS (large incisions, risks of general anesthesia, high infection risk).
This method addresses the problem not by surgically cutting from the “outside,” but by delivering thermal energy “from the inside” through a needle puncture. This is a revolutionary development especially for ulcer patients with compromised skin integrity, because it solves the underlying pressure problem without creating additional trauma to the skin. The procedure can generally be performed under local anesthesia without hospitalization.
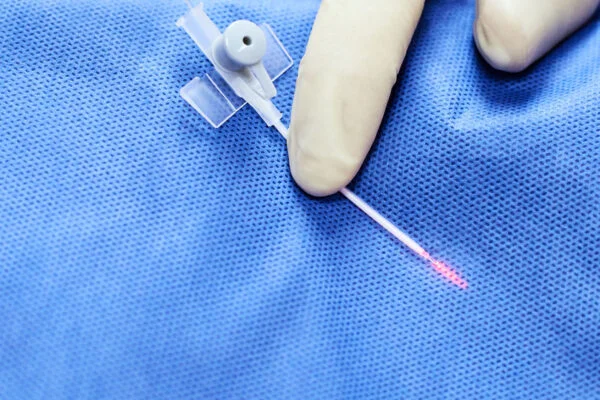
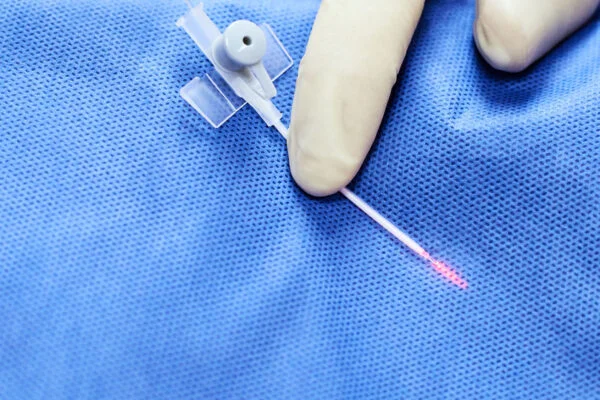
RFA or laser ablation of perforator veins requires a specific technique different from the standard “segmental” ablation used for the major superficial veins (saphenous veins) in the legs. The entire procedure is performed under continuous ultrasound guidance. This method is called the “spot-welding” technique.
Access
The target faulty perforator is identified by ultrasound. After skin preparation, the vein is punctured percutaneously with a fine needle. Through this needle, a special RFA device (stylet) is advanced into the vein.
This is the most important safety step. The active heating tip of the stylet is positioned very carefully to avoid thermal injury to the deep venous system (major deep veins). The ideal position is to keep the tip within the perforator itself, 2.0 to 3.0 mm away from the outer wall of the deep vein. This “safety distance” prevents heat transmission to the deep system.
Once the stylet is correctly positioned, under ultrasound visualization a special fluid (usually a saline solution diluted with lidocaine) is infiltrated into the perivenous tissues around the stylet. This step has two main purposes:
To provide local anesthesia for procedural pain.
To create a protective “heat sink” or “cooling cushion” between the surrounding tissues (skin, adjacent nerves) and the neighboring deep vein. This fluid both physically separates nerves and skin from the heat source and absorbs excess heat to prevent thermal injury (burns) to these tissues.
Perforator ablation uses a static technique known as “spot-welding.” The tip of the stylet is kept fixed at a single location. All four quadrants of the vein wall (anterior, posterior, medial, lateral) are targeted. Each quadrant is treated by applying RFA energy for 60 seconds. This translates to a total ablation time of 4 minutes at a single “spot” location. The goal is not only to shrink the vein but also to create a series of thick, robust, full-thickness fibrotic seals or “plugs” capable of withstanding high-pressure reflux.
After the first “weld” is completed, the stylet is withdrawn by 3 to 5 mm. At this new location, the four-quadrant, 60-second “spot-weld” procedure is repeated. This is continued along the entire length of the perforator (typically from the fascial defect to the superficial vein).
When treatment is complete, the catheter is removed, compression is applied to the treated area, and the leg is wrapped with an appropriate bandage or compression stocking.
RFA treatment of perforator veins has demonstrated both high technical success and satisfactory mid-term durability.
The immediate technical success rate (closure of the target vein during the procedure) is close to 100%. In other words, under ultrasound guidance, closure of the target vein at the time of the procedure is almost always achievable.
Mid-term results are also strong. Foundational clinical studies evaluating the efficacy of fine-catheter RFA or laser show that at a median follow-up of 14 months (approximately 1.5 years), about 82% of treated perforators remain closed (occluded). For a venous segment exposed to continuously high pressures, this is a very robust durability rate.
Yes—this is one of the main goals of the treatment. In patients with ulcers resistant to healing, in whom ultrasound detects underlying perforator incompetence, closing this vein with RFA has a direct positive effect on wound healing. When the underlying high-pressure “jet” stops, the skin tissue finally gets a chance to repair and heal.
Studies report that the vast majority of ulcers in these treated groups heal completely within a defined period. More importantly, recurrence (relapse) is prevented. Analyses show that ulcer recurrence rates decrease significantly in patients who undergo perforator treatment with RFA. This supports that eliminating perforator reflux contributes meaningfully to long-term durability and quality of life in advanced CVD.
In addition to RFA, Endovenous Laser Ablation (EVLA) and Ultrasound-Guided Foam Sclerotherapy (UGFS) are also used for treating perforator veins. Comparative studies have revealed important differences among these modalities in terms of efficacy and safety.
Looking at short-term closure rates, RFA (and other thermal methods such as laser) provides an anatomically superior closure rate compared with UGFS (foam), and this difference is statistically significant.
Even more important is the effectiveness of RFA as a “salvage” procedure. UGFS (foam) has the lowest primary success rate (around 50–60%), and in cases where this procedure fails (i.e., the vein does not close despite foam), secondary intervention with thermal ablation (RFA or Laser) has shown high success rates. The data indicate that RFA is both the primary IPV ablation method with the highest success rate and the most effective rescue treatment for UGFS failures.
What about the clinical outcome—i.e., wound healing? Here there is an interesting nuance. A different study comparing Laser and Foam did not find a statistically significant difference in clinical outcome (ulcer healing time). However, this apparent paradox (similar clinical outcome but different closure rates) is explained by another data point in the study: the UGFS (Foam) group required an average of 1.9 treatment sessions to achieve this outcome.
The clinical takeaway is this: UGFS (Foam) can also achieve ulcer healing, but it is more likely to require repeated procedures to reach that result. RFA is the method most likely to achieve both anatomical closure and clinical resolution in a single procedure (“one and done”).
The safety profile of perforator RFA largely depends on the meticulousness of procedural technique. The main risks and the strategies to mitigate them are directly related; complications are not random but are largely technique-dependent and preventable.
The Instructions for Use (IFU) of dedicated RFA devices specify particular contraindications and risks.
Absolute Contraindication: It is contraindicated to use this device in patients with an active thrombus (clot) visible on ultrasound within the vein segment to be treated.
Potential procedure-related adverse events (complications) include:
The safety profile of RFA depends largely on the operator’s technique (ultrasound proficiency). Almost all of these risks can be directly prevented by two critical procedural steps:
Tumescent anesthesia: infiltration of sufficient “heat-sink” (cooling cushion) fluid into the surrounding tissue. This physically displaces the nerve and protects it from thermal injury, and likewise protects the skin from heat.
Positioning: keeping the catheter tip 2.0–3.0 mm away from the deep venous fascial wall. This “safety distance” prevents transmission of heat to the deep system and thrombosis (DVT/EHIT).
Insufficient or careless application of tumescent anesthesia (heat shield) and catheter positioning (safety margin) are the primary causes of, respectively, nerve/skin injury and thrombotic complications.
Radiofrequency ablation of perforators is applied when the perforator veins located between the superficial and deep venous systems are incompetent, i.e., when they exhibit reflux. It is especially preferred in patients with varicose veins, leg pain, and edema.
In RFA treatment, the problematic perforator vein is heated and closed using radiofrequency energy. Thus, retrograde flow in the vein is stopped, blood circulation is redirected to healthy veins, and symptoms gradually decrease.
Perforator RFA is generally unsuitable for patients with an active infection, a history of deep vein thrombosis, or severe arterial insufficiency. Pre-assessment should be performed under ultrasound guidance.
Patients can usually ambulate the same day after RFA. Mild pain and bruising may last for a few days. Return to daily life is rapid, and full recovery typically occurs within 1–2 weeks.
This method is minimally invasive and does not require incisions or stitches. General or spinal anesthesia is not necessary, and the risk of recurrence is low. It also provides much better cosmetic outcomes than classic surgery.
RFA significantly reduces symptoms by closing the problematic veins. However, depending on the patient’s venous anatomy, new varicose veins may develop. Therefore, follow-up and lifestyle modifications are important.
Yes, the use of compression stockings is generally recommended after the procedure. These stockings support circulation, reduce bruising and swelling, and accelerate the closure process of the veins.
The risk of complications is quite low. In rare cases, a burning sensation on the skin, temporary nerve injury, numbness, or discoloration may occur. When performed under specialist supervision, these risks are minimal.
A closed vein does not reopen, but new perforator insufficiencies may develop in other areas. Therefore, regular surveillance ultrasounds and lifestyle adjustments reduce the risk of recurrence.
Both methods aim to close the vein, but RFA delivers thermal energy more controlled and homogeneously. This translates into less pain, bruising, and tissue damage and a more comfortable recovery.